Platelet concentration is the number of platelets per unit of volume. Usually, platelet concentration is expressed in millions per ml. The platelet concentration factor is the ratio between platelet concentration in PRP and baseline platelet concentration in whole blood and is generally expressed as nX, where n is the value of ratio. When all platelets… Continue reading Platelet concentration & concentration factor
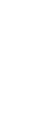
Platelet concentration is the number of platelets per unit of volume. Usually, platelet concentration is expressed in millions per ml. The platelet concentration factor is the ratio between platelet concentration in PRP and baseline platelet concentration in whole blood and is generally expressed as nX, where n is the value of ratio. When all platelets are recovered in the full volume of plasma, the platelet to plasma ratio remains physiological, and the resulting platelet concentration factor is around 1.5-1.7 times the baseline value in blood (1.5-1.7X). A physiological PRP, with recovered platelets of high quality, such as Regen PRP, is relevant for therapeutic use since it respects tissue homeostasis. The clinical results obtained with Regen PRP support this claim (more than 200 published clinical studies, lists available on request).
To get a PRP with a higher platelet concentration, either the full volume of plasma is not recovered, or a volume of the platelet-poor plasma is discarded.
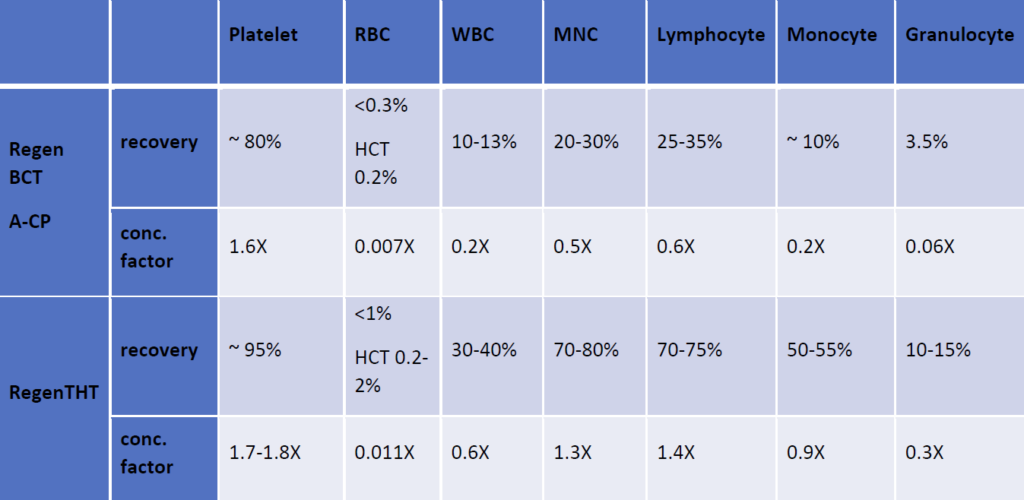
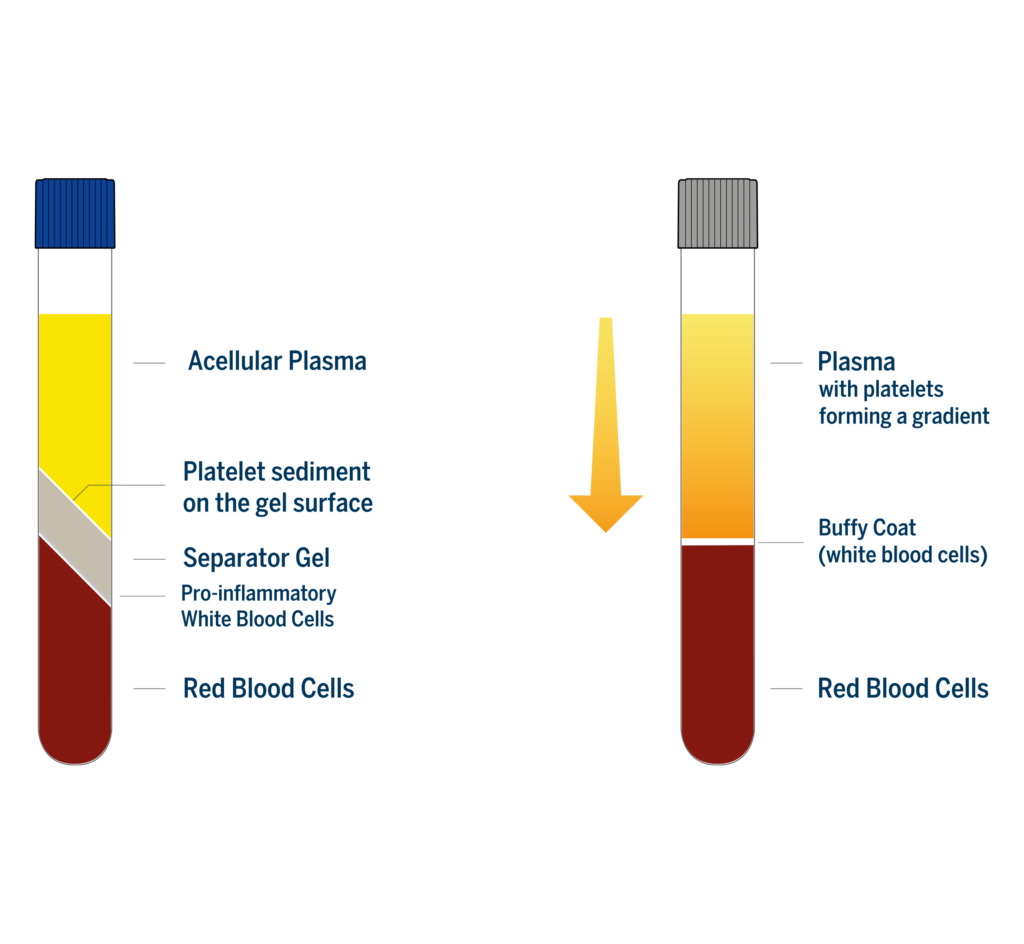
In the case of devices using soft spin centrifugation for the preparation of leukocyte poor PRP such as Arthrex ACP double syringe or Fidia Hy-Tissue there is still some plasma in the red blood cell fraction after the centrifugation. Consequently, the platelet concentration factor can be slightly higher than in Regen PRP, theoretically around 2-3X. Nevertheless, because these devices have no physical separator that isolate the PRP from the other blood components, the composition of the recovered PRP is highly user dependent. This is not the case with Regen Lab technology that produces a standardized PRP. As the separator gel always inserts itself below the platelets and over the red and white blood cells, it ensures a precise blood component separation at the cellular level. All the platelets are recovered over the separating gel at the end of the centrifugation, ensuring a high platelet recovery (>80%), and the physical barrier formed by the separator gel retains the undesired pro-inflammatory white blood cells and the red blood cells in the lower part of the tube.
Due to the low centrifugal force and the short centrifugation time, platelets are still in suspension in the plasma at the end of centrifugation in soft spin devices, instead of being concentrated at the buffy coat level. However, they form a gradient with their concentration increasing toward the buffy coat line.
Most of the operators using soft spin devices stop collecting PRP too hight above the buffy coat line, to avoid the risk of collecting white blood cells. This affect the platelet recovery rate (around 60%), the platelet concentration factor (usually below 2X), but also quality of the recovered platelets.
The densest platelets, which are the richest in growth factors [1] are thus not efficiently collected with this type of technology as these platelets are at the same level as the smallest white blood cells. This can significantly affect the growth factor content of this type of PRP. On the other hand, if the operator goes too close to the white blood cell layer, the resulting PRP will be contaminated with red and white blood cells.
Thus, not only the platelet recovery rate is lower with these soft spin devices, but also, they are not efficiently recovering the platelet fraction that is the richest in growth factors. That means that when compared to Regen PRP with a lower concentration these slightly more concentrated PRP could have the same or even a lower content in growth factors. Tests comparing Regen PRP to Arthrex ACP have shown that when growth factors are evaluated by their total content available in the two types of PRP, all of them were much higher in Regen PRP than in Arthrex ACP (p<0.001) (data on file). In addition, a preliminary report of a comparative study, has shown equivalent clinical results with the two types of PRP on patients suffering from knee OA [2].
For buffy coat PRP a large volume of blood (usually 30 mL or more) is needed to obtain a few mL (3-5 ml) of highly concentrated leukocyte rich PRP. Buffy coat devices use high force centrifugation, thus platelets are at the buffy coat layer at the end of the centrifugation. Because a large part of the acellular plasma is discarded before collecting the platelets, the platelet concentration factor is over 3x. With these devices white blood cells (either all or part of them, depending on the technology of the device) are collected with the platelets and are also concentrated above the baseline value in blood.
A platelet concentration of 1 billion per milliliter, which corresponds to a 4- to 5-fold increase over baseline, is often wrongly quoted as the value for therapeutic PRP. It was first mentioned in landmark publications on PRP by Prof. Robert Marx [3,4] twenty years ago, when the technologies for PRP preparation were rudimentary. This empirical value has never been scientifically evaluated nor has its superiority to lower concentrated PRPs prepared with effective technologies, ever been demonstrated in comparative clinical studies. The technologies used by Prof. Marx in his early PRP studies produced a buffy coat PRP, highly contaminated with red and white blood cells. As these cellular contaminants delay the healing process, a higher concentration of platelets is probably needed in this type of PRP to compensate. A study comparing a 4.7X buffy coat PRP to a 1.5X soft spin PRP showed similar improvements on patients suffering from knee osteoarthritis with the two types of PRP, however, concerning adverse events, more swelling and pain reaction, were found after buffy coat PRP injections[5].
Solange Vischer, MSc. Senior Scientific Advisor
References :